Clinical problem
Physicians integrate large amounts of diagnostic information, including symptoms, medical history, and diagnostic tests, in their decision-making. The diagnostic process requires skills that depend on knowledge, experience and intuition. Despite the availability of diagnostic procedures and tests, many diseases remain undetected until late stage. The main reason is that recognition of combined subtle changes in blood, tissues and organs may elude the attention of the clinician. In particular, patterns in changes in test results will go unnoticed when they do not exceed reference ranges or display clear pathological characteristics. A systematic artificial intelligence (AI) approach to detect patterns in diagnostic test results (laboratory and radiology) that are routinely requested by primary care physicians will (1) assist physicians in interpreting diagnostic data and clinical decision making and (2) enable detection of pathological cases at an early stage.
Solution
This project will focus on development and implementation of an AI-based diagnostic tool. The goal is to assist GP’s in their interpretation and integration of diagnostic data and clinical characteristics of individual patients. This will reduce diagnostic turnaround time and thereby accelerate diagnostics and treatment follow-up. Moreover, case finding by analyzing (retrospective) structured patient data will become possible.
Approach
A practical approach: General practitioners (GP) request laboratory diagnostics and radiology images on a daily basis. As an example, suspicion of liver diseases (such as hepatitis, steatosis, cirrhosis and cancer) is a common reason for requesting diagnostics work up in primary care. The interpretation of test results and the choice of adequate follow up (re-testing, watchful waiting, treatment) is often difficult and may lead to a delay in adequate treatment of the patient. All of the aforementioned liver diseases have their own distinct changes in blood marker and image parameters (including ALAT, ASAT, AF, gGT, bilirubin, CRP, absolute neutrophil count, CT and ultrasound imaging). Using machine-learning, we will integrate the patient’s symptoms, history and diagnostic results to generate an algorithm that predicts the most likely underlying liver disease of the patient (Figure 1). The decision tool will be implemented and the added value in primary care will be evaluated with participating primary care centers. Discovery of the unexpected: The AI based decision tool will be able to recognize unexpected pathology from (patterns of) routinely requested test results. As an example: Approximately 15% of the world’s population suffers from iron-deficiency anemia, which often remains undiagnosed. Cellular blood count and clinical chemistry parameters are often requested as a first orientation when a patient has undetermined physical complaints. These parameters can indicate an iron deficiency, which however often goes unrecognized. Using AI, we will be able to identify iron deficiencies, and additionally provide the physician with advice on follow up or treatment (according to the Dutch NHG guidelines). Additionally, this algorithm will identify undiagnosed haemoglobinopathies or thalassemias.
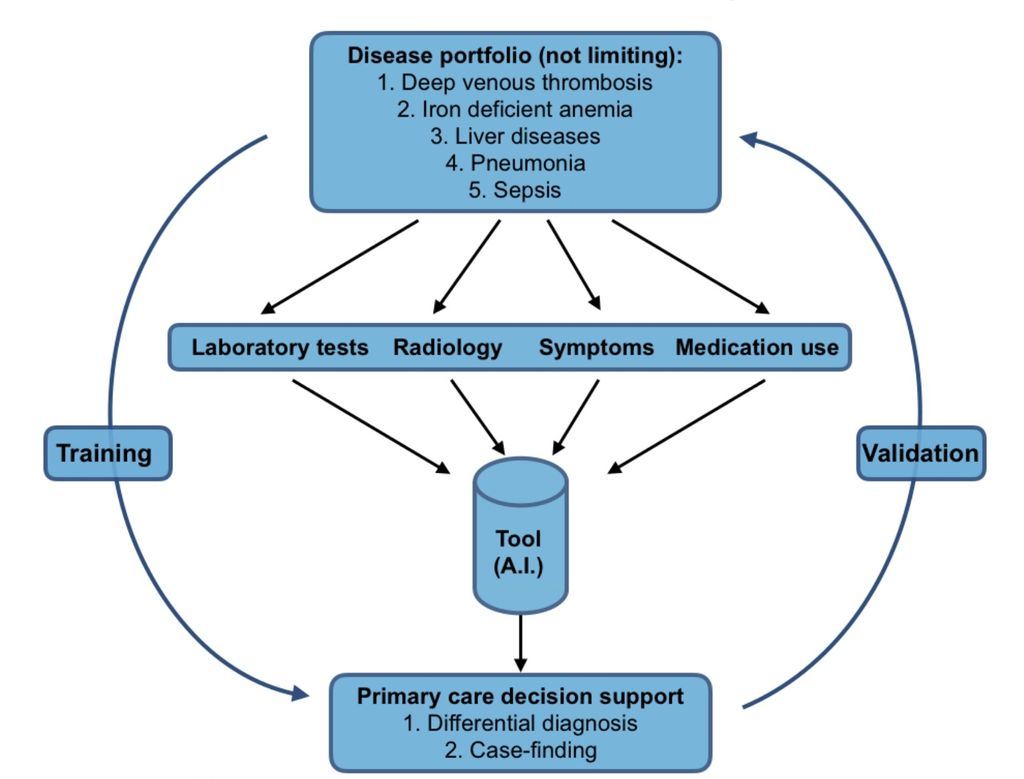 Figure 1. Design of the project
Figure 1. Design of the project




